


Exercise and GLP-1 Medications: Best Practices for Optimal Health
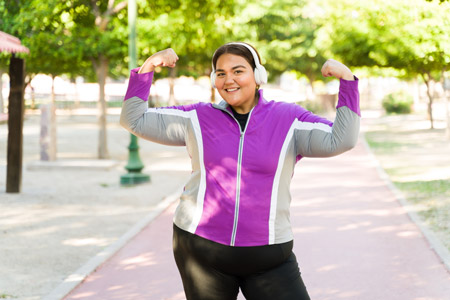
The combination of GLP-1 medications and regular exercise is a powerful duo in the realm of diabetes management. While GLP-1s help improve blood sugar control and promote weight loss, exercise enhances insulin sensitivity, lowers blood sugar levels, and supports overall well-being. When utilized together, these two components create a synergistic effect, leading to improved health outcomes for individuals with type 2 diabetes.
In this article, we'll explore the best practices for incorporating exercise alongside GLP-1 medications, empowering you to maximize the benefits of both in your diabetes management journey.
Let's explore the best practices for integrating exercise with GLP-1 medications:
- Consult with Your Healthcare Provider: Before starting an exercise regimen, consult with your healthcare provider to ensure that it's safe and appropriate for your individual health status and medical history. Your provider can offer personalized recommendations and guidance based on your specific needs and circumstances.
- Choose Activities You Enjoy: Selecting activities you enjoy increases the likelihood of sticking with your exercise routine long term. Whether it's walking, cycling, swimming, dancing, or participating in group fitness classes, find activities that bring you joy and fit seamlessly into your lifestyle.
- Aim for Regularity and Consistency: Consistency is key when it comes to reaping the benefits of exercise. Aim for at least 150 minutes of moderate-intensity aerobic exercise per week, spread out over several days. Additionally, incorporate strength training exercises at least two days per week to build muscle mass and improve metabolic health.
- Monitor Blood Sugar Levels: Regular physical activity can affect blood sugar levels, so it's essential to monitor your levels before, during, and after exercise. Keep a log of your blood sugar readings and note any patterns or trends that may emerge. Adjust your medication regimen and/or carbohydrate intake as needed to prevent hypoglycemia or hyperglycemia during exercise.
- Stay Hydrated and Fuel Your Body Properly: Drink plenty of water before, during, and after exercise to stay hydrated and replace fluids lost through sweating. Additionally, fuel your body with a balanced pre-exercise snack containing carbohydrates and protein to provide energy and support muscle recovery. Be mindful of your carbohydrate intake to prevent blood sugar spikes or crashes during exercise.
- Listen to Your Body and Rest When Needed: Pay attention to your body's signals and adjust your exercise intensity or duration accordingly. If you're feeling fatigued or experiencing pain or discomfort, take a break and allow your body to rest and recover. Overtraining can lead to injury or burnout, so prioritize rest and recovery as part of your exercise routine.
- Be Flexible and Adapt as Necessary: Life can be unpredictable, so be flexible and adaptable with your exercise routine. If you're unable to complete your usual workout due to time constraints or other commitments, find alternative ways to stay active, such as taking short walks during breaks or incorporating physical activity into daily tasks.
The information on this site is for informational purposes only and should not replace direct medical advice, diagnosis, or treatment from your doctor or another qualified healthcare provider.
Sources:
“GLP-1 Agonists.” The Cleveland Clinic.


.jpg)
.jpg)
.jpg)


















.jpg)





















.jpg)

















.jpg)

























.jpg)
.jpg)
.jpg)









